Juliet Gerrard and Rachel Chiaroni-Clarke

NZ bubble cartoon by Mark O’Brien.
As the number of days with zero cases grows, and the chance of successful elimination rises to over 90%, we can begin to collectively breathe out and focus on a return to normal within our New Zealand bubble. With no vaccine or effective treatment on the near horizon, our closed borders remain critical to enable us to relax our restrictions rapidly and prevent a second wave of infection. But loosening control of our borders will also be a critical part of our economic recovery and enable individuals to reunite with friends and family.
It is hard to compromise with a pandemic – we all know now that even a single imported COVID-19 case can create a cluster that quickly spawns hundreds more. So how do we decide to reopen our borders and what constitutes an acceptable level of risk?
Choosing when to open a border
One of the most frustrating characteristics of COVID-19 is the variable and sometimes very long incubation period of the virus. Today’s new case numbers reflect transmission from a couple of weeks ago, so the most up-to-date information on current infections – here and in other countries – may be missing recently emerged clusters and silent chains of transmission that have so far gone undetected. This creates particular challenges in deciding when to reopen the border to specific countries. Our growing understanding of the epidemiology is allowing us to firm up our understanding of how many days a country needs to have had ‘no new cases’ before we can be sure elimination has been achieved. We are looking for needles in a haystack and the difficult question is how long we need to keep looking before we can assume there are none left.
Assuming that high levels of testing are in place, a recent Otago study found that 27-33 days without any new cases means there is a 95% probability New Zealand has completely eliminated the virus. To be 99% sure, we would need 37-44 days. The same study found that with lower testing and fewer people seeking medical help for symptoms, it would take 53-91 days of no new cases to have 95% probability of successful elimination. All these calculations assume that no new cases arrive through the border. So it is important to understand what additional risk is posed if the border requirements change.
Which countries?
As Dr Ashley Bloomfield said recently, “there is still a global pandemic out there.” Most New Zealanders would probably agree that opening the border for quarantine-free travel to all countries would be too high a risk to take in the near future. We would quickly lose gains made and risk going back to square one as new cases trickled in from off-shore – potentially building into a second wave of infections. But the COVID-19 pandemic is playing out in very different ways in different countries around the globe, which may enable us to make some smart choices. At the moment, some places (e.g. Taiwan, Hong Kong, Vietnam and Australia) are managing to stamp out the virus and have, like us, trustworthy testing data that reveals very few known cases. By contrast, other places have sustained community transmission and high caseload numbers (e.g. USA, Brazil and the UK).
This poses many questions: What level of risk are we prepared to take in the face of a potential second wave? When should we allow travel from countries that have avoided any cases altogether? What about those that only had a few sporadic cases and contained them? Or countries that had larger outbreaks but managed to contain and eliminate the virus like we have? And how might we mitigate the remaining risk with appropriate border measures?
The exact criteria for allowing quarantine-free travel to our country are yet to be determined, but some obvious factors to include are:
- The prevalence of active cases. How many cases are there in the country? Where are they on their curve? Does today’s data suggest that prevalence will be low in a few weeks? Has there been community testing to locate undiagnosed cases?
- Confidence in the testing and the data. It is important to look behind the official numbers and be confident that a low case count reflects low cases and not insufficient testing. How many tests are being done? What percentage are positive? What are the types of tests? Is the sample representative?
- Sustained or undetected community transmission. How many people catch it from each person on average (i.e. what is the effective R value)? Are people getting sick without knowing who they caught it from, suggesting a reservoir of undetected cases?
- Confidence in control measures. Are close contacts of a case being rapidly traced and self-isolated to break the chain of transmission? Have previous outbreaks been rapidly controlled? Are the borders open to sudden influxes from other territories?
What are the chances of importing a case?
We also need to think about the probability that a case would actually be imported into Aotearoa New Zealand. The number of travellers has been impacted by the pandemic and the prevalence of cases is likely to change over time. But we can do some simple estimates of how many predicted infected passengers we would introduce if we reopened the border to different countries and pre-COVID traveller numbers returned.
As an example, the US has over 1 million reported active cases. Based on these current statistics, we would expect around 1 in 300 people from US to have COVID-19. If 1000 people were to arrive on our shores each day, we would roughly estimate that there could be three infected passengers from the US every day. This feels like too many, and doesn’t take into account undetected cases not featuring in the US statistics.
By contrast, China currently reports around 70 cases daily, or roughly 1 in 20 million people. If these numbers are stable and accurate, it would be highly unlikely for an infected passenger to arrive this year if 1000 visitors arrived daily. This might be an acceptable risk of known cases. It might be prudent to first understand the degree to which clusters of silent cases are smouldering in regions that previously had high caseloads, especially given the plan for comprehensive population testing in Wuhan is about to be carried out – providing a crucial data set of 11 million citizens to enable undetected cases to be found.
Clearly there is no one size fits all solution.
The need for a nuanced case-by-case solution will need to be offset with the logistical and administrative burden of constant country-by-country risk assessment – in a rapidly changing landscape. We also need an honest assessment of our as-yet-untested response systems to manage a new outbreak.
Are we nimble enough to respond to a rapidly changing landscape?
One thing that we have learned over the last few months is that the situation can change very quickly. Take Singapore, for example: the country had an exemplary initial response but has later had a significant spike in cases. A risk assessment carried out on 22 February, 22 March and 22 April would have given us very different answers. How do we manage this possibility of rapid change, while still giving as much certainty to travellers as possible? How quickly can we manage the transition from quarantine-free travel to requiring quarantine as a backstop in the event of an outbreak, without creating travel chaos?
And how might our risk assessments respond to possible early signs of a second wave? Data from South Korea is interesting here. An impressive public health response got control of the first wave of cases – but at what point in the long tail of cases would we declare travel safe? Is the outbreak in May a blip or the start of a concerning second wave?
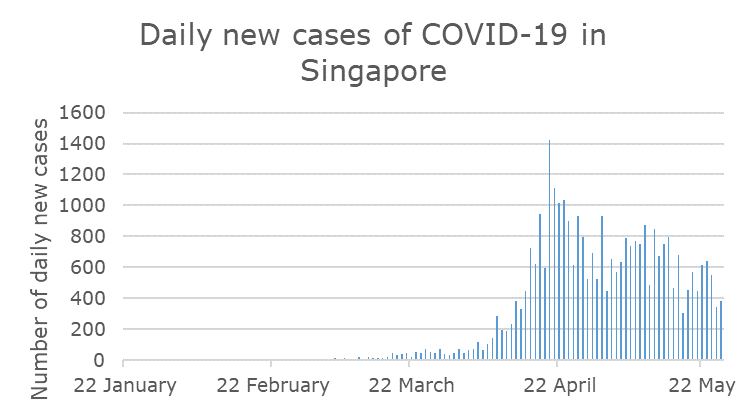
Border restrictions based on case numbers may have exempted Singapore in February and March, but perhaps not in April? And what would we decide in May?
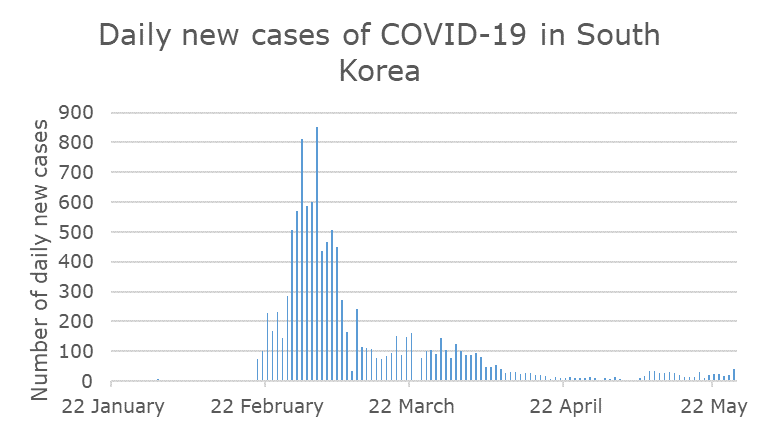
South Korea initially had some of the highest case numbers and therefore posed a high risk for importing cases, but the country has been successful in stamping out the virus and now reports relatively low case numbers. In April things looked safe, but is the outbreak in May a blip or the start of a second wave?
For a few countries in the world which have so far escaped the pandemic, notably in the Pacific, the calculation is relatively simple. In all other cases, if we do open our borders, we need to understand what ‘nearly eliminated’ might mean in countries where the virus has been suppressed. In Australia, some states have had a pattern of zero cases like ours for many days now – suggesting a similar risk profile to us. Elsewhere there is concern that there is still a small but significant low-lying reservoir of the virus that is not being captured in the statistics, but is resulting in some unexplained spikes. New South Wales has been in the news this week with just this scenario. After consistently reported low numbers for weeks, including days with zero new cases, new cases of unknown source have appeared in in the past week. The state closed a school after only reopening for one day after a student tested positive, exposing a new cluster of cases of unknown source. For our trans-Tasman neighbours, we have good line of sight and confidence in the public health systems and we know that testing, tracking and tracing are gold standard. But situations like these will occur all over the world in places where we may have less information from which to estimate how many ‘silent cases’ we might import when we open the borders. These will be highly uncertain calculations.
Can we mitigate the risk with screening and testing at the border?
One way to mitigate these risks is to employ passenger screening to catch cases before they depart or when they arrive. Internationally, this is likely to play an important role for countries to reopen international travel, but no method is perfect. Screening focuses on reducing the risk associated with each individual, as an additional measure after assessing the collective risk from a particular country. There are a range of possibilities here, each with strengths and weaknesses.
- Testing for fever. Screening for high temperatures using thermal cameras or by having their temperature taken manually has the potential to capture people with fever, so that they can be further tested or quarantined. China and South Korea, among others, have used this approach throughout the pandemic, including checking the temperature of passengers arriving at airports. However, while these tests are fast and simple, and do identify some cases, the evidence suggests these tests are not perfect and will only provide accurate results if they are set up and used properly, as detailed in this article in the Conversation. They will not pick up pre-symptomatic or asymptomatic cases, or passengers who have taken medication that lowers fever.
- Virus testing. On arrival or pre-departure, we could require travellers to undergo the same tests we have been using throughout the pandemic to check a person is virus-free. There may be limitations in the turnaround time for results (at least a few hours, currently) and capacity to cater to tourist numbers, in terms of test kit supply, but this approach is being used in a few countries internationally. Currently anyone arriving into Austria has to provide a medical certificate proving a negative COVID-19 test result that cannot be older than four days. People can also pay for a test at the Vienna airport, with results available within about three hours. Cyprus is using a tiered approach with travellers from some countries deemed lower risk not requiring proof of being virus-free but those from countries with more cases needing to show a health certificate. Iceland is ironing out procedures for testing on arrival and use of a contact-tracing app to provide information to tourists, before easing quarantine requirements. This is a surer method than testing for fever, but pre-symptomatic cases may still slip through the net.
- Antibody testing. These tests have the potential to reveal who has been exposed and might now be immune to COVID-19, but are not yet reliable enough to be used for this purpose. Limitations include a lack of evidence that a positive antibody test means that someone is not infectious, and a negative antibody test does not mean the person is virus-free.
A combination of testing for fever, interviews at the border, and the standard PCR test either prior to departure or on arrival would go a considerable way to reducing the risk of importing cases, but not provide a full guarantee.
Breaking the chain of transmission if border control fails needs ever stronger testing and tracing
Despite reducing risks by limiting who has access to quarantine-free travel, when they can enter, and undertaking individual screening upon arrival, there is still a chance cases will be imported. Detecting these cases rapidly is vital to containing the spread of any new cases and maintaining elimination of the virus, and we must do this without the tools for widespread surveillance which have been deployed in places where there are fewer concerns about individual privacy. This requires ongoing widespread surveillance testing of the New Zealand population, including broad testing of people displaying any of the wide-ranging symptoms associated with COVID-19.
A second recent Otago study modelled how long it might take to detect an outbreak if a case were imported and how many cases we would have by that time. They found that we could detect 95% of outbreaks up to 33 days after introduction, by which time there would be between 1 and 68 infected cases in the community. To pick this up, we would need to be doing around 5600 tests a day, mostly focused on people who present to their GP or hospital with symptoms. These estimates assumed Level 2 measures and more tests would likely be required, with well designed surveillance and geographical spread, once we are at Level 1. This highlights that the combined risk of moving to Level 1 and selected border openings would require particular caution, increasingly strong surveillance testing and readily available surge capacity for contact tracing in the case of a second outbreak in Aotearoa New Zealand.
Expanding international bubbles
As reported in The Guardian, the leaders of several countries including New Zealand and Australia “agreed that as each begins to ease restrictions they could capitalise on low infection rates by creating tourism safe zones.” Greece has already released a list of countries, including New Zealand, from which it deems visitors to be coming from an epidemiologically safe place. The Straits Times also reported that China is opening up its borders to a range of countries with very different epidemiological profiles – Singapore, Japan, Britain, Germany, France, Italy and Switzerland, and maybe others. Preventing crossover between low and higher-risk zones will be important to avoid possible reintroduction of the virus to places where it is contained or eliminated. The rules around passengers from high-risk countries transiting through low risk countries in our bubble will need careful attention.
All things considered, we can have some cautious optimism that international travel between safe countries will soon start to be possible. It will take a carefully managed and nimble process: identifying low-risk countries, monitoring for stable low case numbers, and perhaps testing individuals on arrival. Finally, we need to ensure that we are ready to act if we detect an outbreak, and quickly suspend any arrangements that are not protecting us from new cases, as we cautiously expand our bubble beyond Aotearoa New Zealand’s borders.
This article has been republished with permission on the New Zealand Herald website
